In Vitro Fertilisation with donor sperm
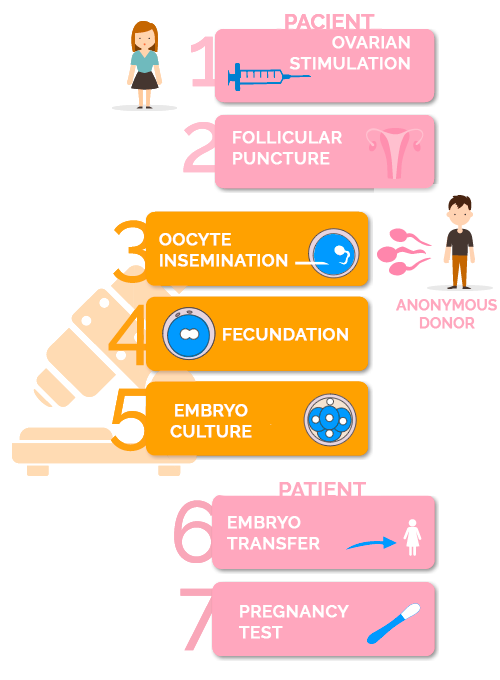
In vitro fertilization (IVF) with donor sperm is a technique by which the oocytes, once extracted by follicular puncture, are fertilized in the laboratory by the sperm of a carefully selected anonymous donor. Those that are fertilized correctly are monitored for several days until the best quality embryos are transferred to the maternal uterus. It is the most widely used assisted reproduction technique, thanks to its high pregnancy rates.
What is In Vitro Fertilisation (IVF) with donor sperm?
For whom is this technique indicated?
In Vitro Fertilisation with donor sperm (heterologous IVF) is indicated for
- Couples where the man has severe male factor infertility, with poor sperm quality or azoospermia.
- Couples where the man is the carrier of a genetic disease that cannot be diagnosed by PGD (Preimplantation Genetic Diagnosis).
- Couples where there is suspicion of poor embryo quality or repeated implantation failures due to a male factor infertility as the main cause.
- Couples who have failed prior In Vitro Fertilisation with the partner’s semen.
- Women without a male partner who want to get pregnant and be single mothers
- Couples of homosexual women.
The requirements for a couple to undergo in vitro fertilization and have the best chance of success are:
- The use of an ultrasound scan to rule out possible uterine malformations that could affect the implantation and development of the pregnancy. In addition, to guarantee a response to ovarian stimulation to recover a minimum of oocytes suitable for the performance of the technique.
- To select a semen sample from an anonymous donor bank with adequate count and motility parameters, selected with a “Donor Screening” protocol that detects autosomal recessive genetic diseases.
Where do sperm donors come from?
Semen donors, according to the Spanish legislation on donations, must meet certain requirements. They must be between 18 and 35 years old, in good mental and physical health, have good semen quality and not suffer from any genetic or sexually transmitted disease.
VITA uses the CEIFER sperm donor bank, whose donors go through a strict and exhaustive examination in order to guarantee the quality of the treatments. The donor will undergo various tests and studies, such as a first medical evaluation, a psychological test, a study of the sperm quality, a genetic study and a study of infectious diseases, sexually transmitted diseases, etc.
All sperm donors go through the “Donor Screening“, a Study of Autosomal Recessive Genetic Diseases Carriers. Through this test it is possible to detect the most common autosomal recessive genetic diseases. In addition, when the time comes to assign the donor, a “Genetic Matching” protocol is followed, so that the donor and the patient do not share mutations in the same genes.

